Our Location
304 North Cardinal St.
Dorchester Center, MA 02124
Due to its powerful antimicrobial activity, silver is a commonly used adjunct product in wound care. However, it also has the potential to impair healing by exerting toxic effects on keratinocytes and fibroblasts. The conclusions of the published literature on the use of silver in wound care vary widely, making it difficult to develop useful treatment guidelines.
Although there is some evidence to support the short-term use of dressings containing nanocrystalline silver in infected wounds, the use of silver-containing dressings in cleaning wounds and closing surgical incisions is not recommended. Negative pressure wound therapy can accelerate the healing of contaminated wounds, especially when silver is used as an adjunct. For burns, silver sulfadiazine can slow healing and should not be used. Instead, alternatives such as nanocrystalline silver or octenidine and polyhexane produced fewer infections and faster healing.
In infected wounds, silver is beneficial for the first few days/weeks, after which a non-silver dressing should be used instead. For clean wounds and closed surgical incisions, silver offers no benefit. The ideal silver formulation is nanocrystalline silver and silver-coated polyurethane sponge for negative pressure wound therapy. Silver sulfadiazine impairs wound healing. Proper use of silver-containing dressings is essential for optimal wound healing.
Over the past few decades, there has been a renewed interest in silver as a topical antimicrobial. Silver sulfadiazine (SSD) is a very widely used silver preparation, especially in burns. In addition, dressings with nanocrystalline silver have also been developed. These new dressings continuously release silver ions into the wound.
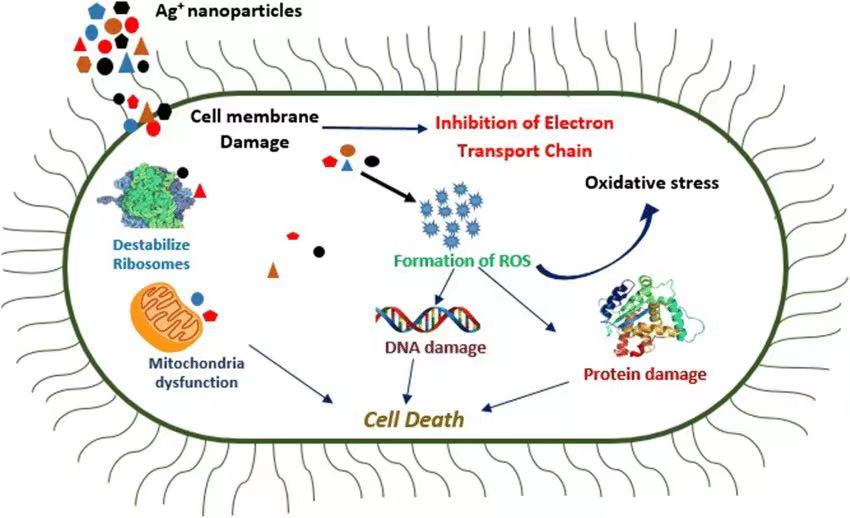
Although silver ion has excellent antibacterial and bactericidal properties, it is also toxic to fibroblasts at high concentrations. Improper use of silver-containing dressings can lead to impaired wound healing. Therefore, guidelines for the proper use of silver-containing dressings must be developed.
The purpose of this study was to assess the available evidence for the use of silver in wound care. We try to answer the following questions:
1) What is the quality of the published research on the use of silver in wound care?
2) What are the advantages and disadvantages of various silver delivery systems?
3) What is the evidence for the use of silver-containing dressings in infected and heavily contaminated wounds?
4) What is the evidence for the use of silver-containing dressings in clean and decontaminated wounds?
5) What is the evidence for the use of silver dressings in burns?
6) What is the evidence for the use of silver dressings on closed surgical incisions?
7) What is the best strategy for using silver dressings?
8) How does silver compare to other, lesser-known formulations?
Silver formulation, effectiveness and toxicity
Although silver ion is a very powerful antiseptic, it also has systemic and local toxic side effects. Systemic toxic effects are due to the absorption of silver through wounds, resulting in argyria (Argyria), manifested as irreversible gray skin discoloration and loss of night vision. 13–15 However, systemic toxicity is rare because serum silver is rapidly excreted in urine and feces.
The local toxic effects of silver are more likely to occur due to the cytotoxicity of silver ions on keratinocytes and fibroblasts. Poon et al. found that silver was cytotoxic at concentrations of 33 ppm or higher in monolayer cultures of keratinocytes and fibroblasts. 16 However, when fibroblasts were cultured in collagen scaffolds, which better replicated in vivo conditions, the toxic concentration was increased to 60 ppm. On the other hand, for silver ions to have effective bactericidal activity, a concentration of 30 to 40 ppm is required.
Therefore, an ideal silver-containing dressing should maintain sustained (several days), therapeutic (≥30 ppm) silver ion concentrations in the wound without causing systemic or localized (≤60 ppm) silver toxicity.
The new dressings containing silver in the nanocrystalline state can elute silver into wounds in a sustained manner, maintaining concentrations of up to 70 ppm (slightly above the toxicity threshold for keratinocytes and fibroblasts) for several days. 16 These newer formulations include Silverlon (silver-coated nylon, Argentum Medical, Geneva, Ill), Acticoat (silver-coated polyethylene, Smith & Nephew, London, UK), Mepilex Ag (silver-coated foam, Mölnlycke Healthcare, Norcross, Ga.), Mepitel Ag (silver-coated silicones, Mölnlycke Healthcare, Norcross, Ga.), Aquacel Ag (silver-coated hydrophilic fibers, ConvaTec, Reading, UK), Promogran Prisma Ag and V.A.C. GranuFoam Silver (silver Coated Polyurethane Sponge, KCI, San Antonio, TX), etc.

Each of these formulations has advantages and disadvantages: Acticoat tends to stick to the wound bed and can be painful to remove,unlike Mepitel Ag and MepilexAg, both have a silicone surface that allows them to blend with surrounding Normal skin adhesion, but not the wound itself. Promogran Prisma contains collagen that acts as a sacrificial matrix for matrix metalloproteinases (MMPs) to enhance wound healing. 20, 21 Silver-coated polyurethane negative pressure wound therapy (NPWT) sponges combine the advantages of NPWT with sustained release of 20 to 40 ppm of silver, 22, 23 at concentrations below the toxicity threshold for keratinocytes and fibroblasts.